Introduction
Success in pediatric dentistry is based on the ability to control the child. The kind of communication during treatment is one of the major differences between adults and pediatric dentistry.
In general, a special relationship might be existed between dentists, and both children and parents during dental treatment[1]. Behavior management is widely agreed to be a key factor in providing dental care for children. In fact, if a child's behavior could not be managed during dental treatment, it would be difficult, if not impossible, to carry out any dental care [2].
Psychological and behavioral findings indicate that local anesthetic injection, placing rubber dam, and starting tooth preparation using high speed hand piece are the three most frightening dental works that make the child anxious.
On the other hand, fearing from anesthetic injection results in anxiety and fearing from dental treatment in a large number of children provokes inappropriate behavioral reactions.
Furthermore, it was studied whether age, previous dental experience, level of dental anxiety and injection site affect the self-reported pain of children during the first and second treatment sessions. After receiving a local anesthetic injection and prior to dental treatment, patients were asked how much pain did they experience.[3]
General anesthesia (DGA) is the only available option to facilitate performing dental treatment in anxious children, This technique must be carried out in a professional environment by an expert and well trained team who are able to comply with the recommendations for alternative sedation techniques[4].
Natural fearing from intensive light, loud sound and sudden strange movement results in stress easily. The most anxiety induced behavioral reaction is shown by children in their first three years of life.
In general, two groups of behavior controlling methods are available. The use of pharmacological agents such as sedatives, nitrous oxide, general anesthesia etc.[1],[5],[6] and behavioral psycho therapy techniques, relaxation and hypnotherapy which are recently assumed to have an increasing prominence as the effective treatment regimes.
Many dentists currently provide pediatric dental treatments under intravenous conscious sedation[7]. Yasny et al suggested, consequently, pre-operative pharmacological intervention may be necessary, Enteral sedation may be the optimal adjunct for such a challenging patient[8].
Dentists have used a number of methods of hypnosis to manage dental phobia disorders [9],[10]
Hypnosis is a state of altered consciousness in which the patient’s awareness of surrounding world including somatic sensations turns to awareness of a more comfortable world within his/her mind. The hypnosis technique described here, is very useful to break the phobic cycle of anxiety and fear.
Estimations have shown that significant number of people experience fear and anxiety during dental treatment[11]. The patient’s fear from dental treatment is cultural . Hypnosis may be the method of choice in patients who reject or cannot receive pharmacological modalities, or behavioral interventions. Hypnosis is a state of mind in which suggestions are not only more readily accepted than in the waking state, but also are being put into action upon a much more powerful fashion than would be possible in normal conditions[12].
Reports indicate that while 40% of the population of the world experience fear of dentistry but only 5% is related to true phobia[13].
Pathological dental phobia is characterized by the avoidance of dental treatment in addition to a high level of anxiety[14],[15]. Dental phobia can be classified as a
specific phobia according to DSM IV because it demonstrates the following characteristics[16]:
The person is inconstantly frightened from described stimuli.
Confronting the specific stimulus provokes an almost immediate and unpreventable fear reaction.
The triggering stimulus is usually avoided,
The person’s daily routine is greatly affected by anxiety or avoidance pattern.
The person realizes that his/her fear is unreasonably exaggerated.
Attempts to assess dental fear have been mainly considered in the purpose of researches. Numerous published studies, collected data of self reported dental anxiety as the primary outcome variable. To assess various anxieties for example, indicators of pre and post treatment level of anxiety have been considered in data collection[17].
Most of the studies about the techniques of management are published by the specialized dental anxiety clinics in America[18], Sweden[19] and Netherlands [20], but rarely by UK dental practitioners [21].
Kvale et al in a meta- analysis concluded that about 80% of participants in the experiment might receive conventional dental care, but they were wondering if the results could be generalized to all patients[13].
Materials and Methods
The present study was conducted in the department of oral medicine and diagnosis, school of dentistry, Isfahan University of medical sciences, Isfahan, Iran, 2007. Specific requirements, other than dental equipments and instruments, were a relatively quiet environment for hypnosis and patients’ cooperation. In the process of patient selection, thirty children with age range of 8 to 12 years and equal sizes of both sexes were selected. Short explanation was given to the patients and their parents about voluntarily participation in this study. Then, the parents were asked to announce their consent to dental treatment and hypnotherapy.
The patients who did not accept the procedures including anesthetic injection and hypnotherapy and those who had a history of nervous system or mental disorders were excluded from the study. In this crossover study half of the patients received hypnotherapy prior to anesthetic injection in their first session of treatment and only injection in the second session. The order of process for other half was inversely. Then a comparison between two groups was made.
In this study, the physician and the medical care team were the same in both groups and also other conditions, such as visiting duration which were tried to be kept identical.
It was needed to communicate briefly to patients before hypnosis and this had to be done very carefully, of course.
In this way, physician had the opportunity to assess the patients’ imagination about this process and also psychological factors affecting hypnotherapy including patients’ calmness versus anxiety, patients’ confidence, paying attention to different stimuli including verbal and visual ones , attention span and response.
When the patient was sitting quietly in semi-fowler’s position and was relatively calm, hypnosis was started.
The hypnosis technique in this study was selected based on the literature . In this technique, a combination of fixed looking method, counting, and imagery which is a helpful combination for children was used. During local anesthetic injections, observations were recorded intermittently.
At the end of injection, the observations during anesthesia including patient’s pulse and respiratory rates; behavioral reactions such as crying, hands or feet movement, physical strength, response to speech and oral- physical resistance were recorded by two persons.
Following appropriate inculcation, injecting local anesthetic agent, and returning oral and maxillofacial position to normal, it was time to wake the patient up gradually and talk briefly to assure him / her about having no pain because of successful local anesthetic injection.
Observations were recorded for all patients for both hypnotic and non- hypnotic states.
Conclusion
After passing through practical phases on the 30 subjects and recording their behavioral reactions, data were analyzed (Table 1). The statistical method in this study was MC.Nemar`s analysis and the method of data collection was sequel sampling. Fifteen patients received hypnotherapy in their first visit and the other 15 in their seconds.
Findings showed that during local anesthetic injection heart and respiratory rates were less than normal in hypnotic group and there was a significant difference between two groups. These findings indicated that hypnosis reduced adverse and unfavorable reactions therefore was successful (Table2).
Behavioral reactions of two groups were compared and the results are reported in (Table 3). Seventeen out of 30 subjects did not show crying reaction, 8 subjects cried in non hypnotic anesthetic injection state, but they did not do so in hypnotic state; 3 subjects cried in both methods and 2 subjects cried in hypnotic state and did not do so in normal state (p=0.109).
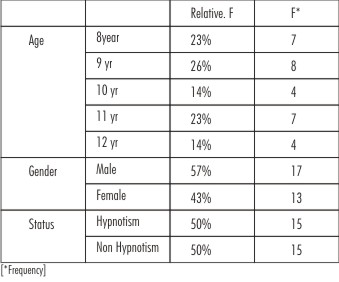 | Table No : 1
 |
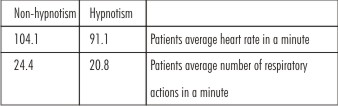 | Table No : 2
 |
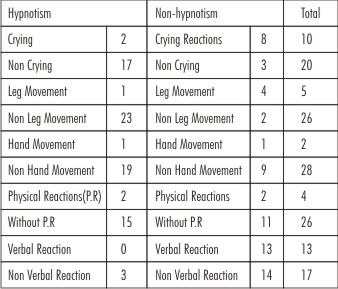 | Table No : 3
 |
Twenty three subjects had no feet movement reaction during anesthetic injection, 4 subjects had normal response while they showed negative reaction in hypnotic state, 2 subjects had positive reaction in both methods and only one subject had positive reaction in hypnotic state and did not have any reaction in normal state (p=0.375).
Ninteen subjects had no hand movement reaction, one subject showed hand reaction in both methods, 9 subjects had hand movement in normal state while they had no response in hypnotic state and only one subject had hand movement in hypnotic state (p=0.021).
Fifteen subjects did not show any physical resistance to anesthesia, 11 subjects showed a normal response while they did not do so in hypnotic state. Two subjects showed resistance in hypnotic state and only 2 subjects showed resistance in both methods (p<0.022).
Adverse oral reactions (p = 0), and physical-oral response (p =0.021), were showed in two cases of injection alone. The majority of patients in hypnotic state showed favorable reactions.
Discussion
Findings showed that the difference between both crying and feet movement reactions in two groups was not statistically significant, but, there were significant difference between other indices.
Regarding our general and specific goals, it can be concluded that the total incidence of adverse reactions during local anesthetic injection was significantly lower in hypnotic state in compare to injection alone.
Hypnotherapy, according to the observed physiological & behavioral statuses of patients, could be used as a treatment method during local anesthetic injection for 8 to 12 year old children.
However, other specific and experimented techniques for behavioral control might be used with hypnosis.
According to the findings of the present and previous studies, hypnosis might be selected by dentists and physicians as an acceptable solution.
Allen & Stanley expressed that traditional behavioral management techniques such as tell- show- do restraint, hand over mouth exercise and sedation were better than the new ones including modeling and contingency management[20].
Among subjects, there were some who did not respond to usual method of behavioral controlling, this might have a root in previous fears, anxieties & dental operations.
Intercultural studies showed that women’s level of anxiety is more likely to have a constant value, while men showed a wide range of responses for a level of anxiety due to their culture[23],[24]. A direct relationship between low socioeconomic status and low oral hygiene and consequently more likely to have missed, damaged or decayed teeth has been shown[25],[26]. Therefore these people might have more reasons to fear from dental treatment, but regarding their educational status, no statically significant differences were found.
One special need that many patients have is treating in a way with no or decreased dental fear. While pharmacological- sedation methods are absolutely vital for compassionate and effective treatment of these patients, there are other important & helpful modalities. The first and the most practical method is good communication to calm down all dental patients[11].
Dailey et al[21] showed that dental practitioners involved in dental anxiety issues were unlikely to use any formal method of assessing dental anxiety. During dental treatment, pain is increased by anticipation and fear, and the majority of hypnosis efficacy is attributed to probably reducing non-specific anxiety.
Orne stated” hypnosis has been shown not to be an effective means of causing an individual modify the behavior that he is not ready or willing to modify"[27].
The effectiveness of hypnosis depends not only on the skill of therapist but also the ability of patient to receive the induction[28].
On the other hand, physical, mental and emotional status and hypnotic nature produce tranquility and favorable state. Memories of the treatment free form mental stress or anxiety which may accompany the treatment. Substantial clinical studies demonstrate that hypnosis effectively reduces anxiety, enhances coping, and has been used successfully to treat behavior disorders, school phobias, and sleep disorders. Hypnosis can effectively reduce a child's anxiety and symptoms and has few side effects when used competently[29].
References
1. right,GZ.Psychologic management of children`s behaviors.In:MCDonald,REAvery ,DR.dentistry for the child and adolescent.7 th ed.St.Louise :Mosby,2000:34-51.
2. Valente SM.Clinical hypnosis with school-age children. Archives of Psychiatric Nursing. 1990:4; 131-136
3. Versloot J, , Veerkamp JS, Hoogstraten J. Children’s self-reported pain at the dentist. PAIN J , 2008;137(2) :389-394
4. Hand D, Averley P, Lyne J, Girdler N. Advanced paediatric conscious sedation: an alternative to dental general anaesthetic in the U.K. SAAD Dig. 2011 Jan;27:24-9.
5. Smyth J. A Program for th treatment of sever dental fear.Report of three cases, Aust Dent J, 1999 , Dec , 44(4) :275-8.
6. Noble,S. The management of blood phobia nad a hypersensitive gag reflex by hypnotherapy: a case report,Dent update, 2002, Mar, 29(2): 70-4.
7. Robb ND, Hosey MT, Leitch JA. Intravenous conscious sedation in patients under16 years of age. Fact or fiction?. Br Dent J. 2003 May 10;194(9):469-71.
8. Yasny JS, Asgari A.. Considerations for the use of enteral sedation in pediatric dentistry. J Clin Pediatr Dent. 2008 Winter;32(2):85-93.
9. Corah NL, Pantera RE. Controlled study of psychologic stress in a dental procedure. J Dent Res 1968;47:154-157.
10. Scott DS, Hirschman R . Psychological aspects of dentl anxiety in adults. JADA1982;104:27-31
11. Peltier B , Psychological treatment of fearful and phobic special needs patients , Spec Care Dentist 2009; 29(1): 51-57.
12. Peretz B. Confusion as a technique to induce hypnosis in a severely anxious pediatric dental patient. J Clin Pediatr Dent. 1996 ;21(1):27-30.
13. Kvale G, Berggren U, Milgrom P. Dental fear in adults: a meta-analysis of behavioral interventions. Community Dent Oral Epidemiol 2004;32: 250-64
14. Johren P, Margraf-Stiksrud J: Zahnbehandl ungsangst und Zahnbehandlungsphobie bei Erwachsenen.Stellungnahme der DGZMK. Deutsch Zahnarztl Z 2005; 57:9-10.
15. Slovin M, Managing the anxious and phobic dental patient. NY State Dent J. 1997;63:36–40
16. Jackson C, Lindsay S. Reducing anxiety in new dental patients by means of leaflets. Br Dent J 1995; 179: 163-167.
17. Diagnostic and statistical manual IV: diagnostic criteria From DSM-IV. American Psychiatric Association, Washington D.C.1994,
18. Milgrom P, Weinstein P. Dental fears in general practice: new guidelines for assessment and treatment. Int Dent J 1993 ; 43: 288-293
19. Johansson P, Berggren U. Assessment of dental fear. A comparisom of two psychometric instruments. Acta Odont Scand 1992;50”43-49.
20. Johansson P, Berggren U, Hakeberg M, Hirsch JM. Measures of dental beliefs and attitudes : their relationships with measures of fear. Community Dent Health 1993; 10: 31-39.
21. Dailey Y M, Humphris G M, Lennon M A. The use of dental anxiety questionnaires: a survey of a group of UK dental practitioners. Bri DenT J 2001 ; 190(8):540-543
22. Allen KD, Stanley RT, McPherson K. Evaluation of behavior management technology dissemination in pediatric dentistry. Pediatr Dent. 1990; 12: 79-82
23. Fuks AB, Steinbock N, Zadik D The influence of social and ethnic factors on dental care habits and dental anxiety: a study in Israel. Int J Paediatr Dent 1993;3:3–7
24. Schwarz E, Birn H. Dental anxiety in Danish and Chinese adults—a cross-cultural perspective. Soc Sci Med 1995:41:123-130
25. Mehrstedt M, Tonnies S, Eisentraut I.Zahnbehan-dlungsangste, Gesundheitszustand und Lebensqualitat.Verhal tenstherapie und Verhaltensmedizin 2002; 23:329–340
26. Wetzel W-E, Hüge I,Ehret R Soziostrukturelle Einflüsse auf die GebiSgesundheit13-14jahriger Schulkinder.Dtsch Zahnarztl Z.1984 ;39:456–460
27. Orne MT,Dinges DS: Hypnosis, in Wall PD ,Melzack R(eds):Textbook Of Pain.Churchil Livigsone,1984,P 806.
28. Goldman L. The Mathematcs of Hypnosis and Pain. Anesth Prog 1989;36: 201-209
29. Roberts JF, Curzon ME, Koch G, Martens LC. Review: behavior management techniques in paediatric dentistry. Eur Arch Paediatr Dent. 2010 Aug;11(4):166-74.
|